Postpartum Depression (abbreviated PPD) is a maternal mental illness that affects women after child birth. According to Postpartum Support International (PSI), Postpartum Depression affects up to 15% of all new mothers. These rates are thought to be higher in developing countries such as Kenya, making PPD one of the most common complications in the perinatal period.
The birth of a baby is known to elicit a wide range of emotions. These include exhilarating joy, excitement at the thought of been a mother, anxiety about the future and even fear. For some moms however, it leads to baby blues and/or Postpartum Depression.
What are the baby blues?
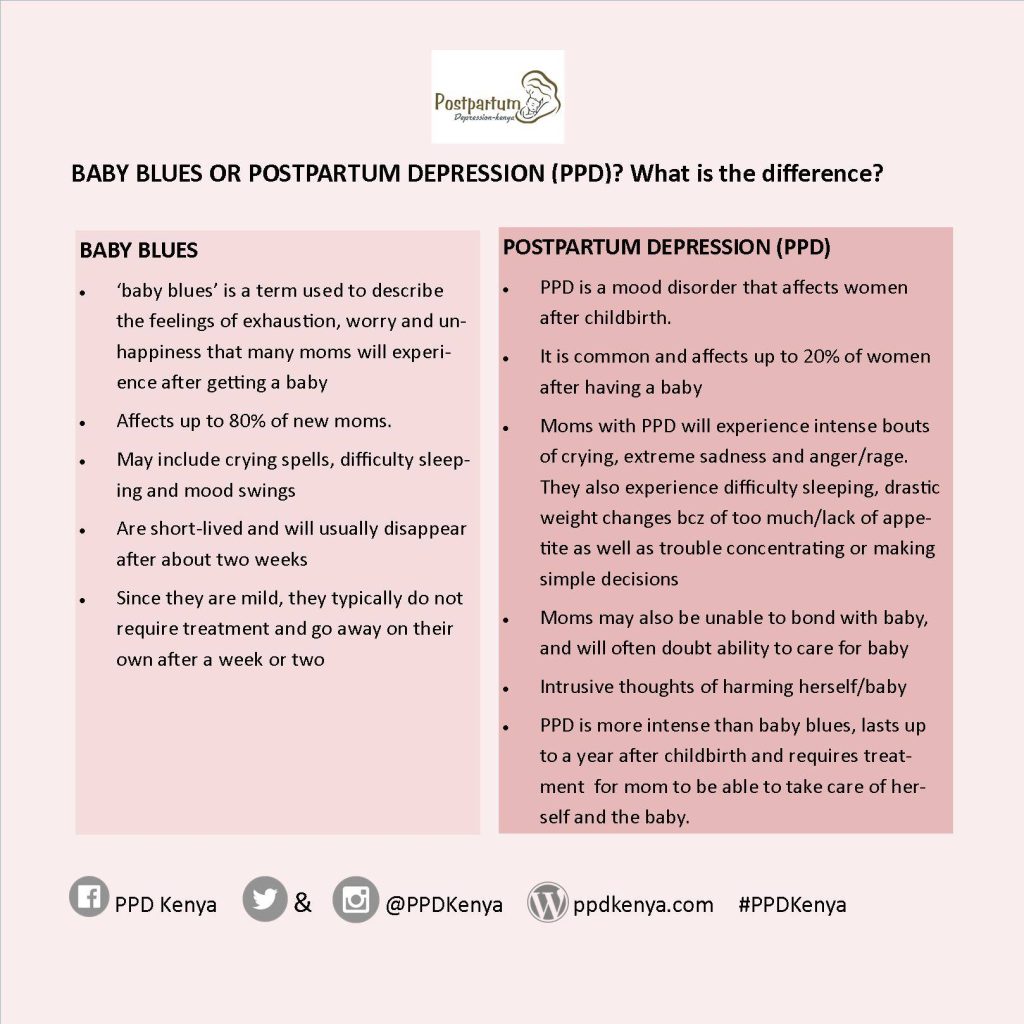
The American Pregnancy Association defines baby blues as a mild condition that affects up to 80% of new moms. The baby blues set in a few days after delivery. The precise cause of the baby blues is unknown, but research shows that this could be linked to the sudden hormonal changes in the body.
In addition to the hormonal changes, a new mother has to make adjustments that often interfere with their sleep patterns and daily routine. All these changes can contribute significantly to how a new mom feels.
Some of the symptoms of the baby blues include:
- Feeling teary
- Inability to sleep even when the baby is sleeping
- Exhaustion
- Poor concentration
- Excessive worrying
- Feeling sad
How long do the baby blues last?
The baby blues are typically mild and short-lived. For the most part, they last up to a few hours a day, and often disappear on their own within about two weeks. For this reason, the baby blues do not usually require medical intervention.
The baby blues and Postpartum Depression
Unlike the baby blues, Postpartum Depression is more intense, and does not usually go away on its own. It is not easy, however, to always tell the two conditions apart. This is because at the onset, Postpartum Depression presents similarly to the baby blues. The two conditions share some of the symptoms, making it harder for many new moms to distinguish the two.
The key difference between the baby blues and Postpartum Depression lies in the severity and how long the condition lasts. The Postpartum Support International website highlights that the symptoms of Postpartum Depression begin after birth, and may last up to one year postpartum. Unlike baby blues which are mild and last up to two weeks, Postpartum Depression is more intense and lasts up to a year after birth.
What are the symptoms of Postpartum Depression?
In addition to the symptoms of baby blues, Postpartum Depression symptoms also include:
- Inability to bond with the baby
- Feelings of intense anger/ rage
- Appetite changes (too much appetite or lack of appetite)
- Sleep disturbances (Insomnia or hypersomnia)
- Loss of pleasure in activities that a mom previously enjoyed
- Weepiness
- Feelings of shame, worthlessness and guilt
- Intrusive thoughts
- Escapist thoughts (these are thoughts of getting away or travelling to a far place not wanting to come back)
- Thoughts of harming the baby and/or self-harm
- Suicidal thoughts
It is important to mention that these symptoms differ from one mother to another. One mom may have just a few symptoms while another may have almost all the symptoms listed above for Postpartum Depression.
Risk factors for Postpartum Depression
Risk factors are defined as factors that predispose a woman to Postpartum Depression. One of the key risk factors is a history of Postpartum Depression. A woman who has had PPD before has a 50% risk of getting the condition again in subsequent births. Other risk factors associated with Postpartum Depression include:
- A history of mental illness in the family
- Unwanted/ unplanned pregnancies
- Inadequate support for the new mother
- Significant life events at the time of pregnancy and/or birth, such as retrenchment, death of a loved one or relocating to a new town
- Financial constraints that make it hard to care for the baby
- Conflict in relationship/ marriage
- Complications during pregnancy and/or the birth process
- Complications with breastfeeding
- Getting multiples (twins, triplets, quadruplets etc)
- Mothers whose babies are born and taken to the Neonatal Intensive Care Unit (NICU) are also at risk of PPD
- Mothers who have gotten pregnant following infertility treatment have also been shown to be at risk of PPD
- Mothers who get babies with special needs
It is important to be aware of these risk factors. Research indicates that all of the factors listed above put pregnant women and mothers at a higher risk of Postpartum Depression and other maternal mental illnesses. Additionally, if one presents any of these factors, it is important to speak to a healthcare provider. This is helpful because it allows the woman to plan ahead for assistance and care if need be.
Treatment options for Postpartum Depression
Postpartum Depression is temporary provided affected mothers get professional help. Treatment options available for Postpartum Depression depend on the severity of the condition. Baby blues are mild, and mothers will usually recover with adequate support from family, getting enough rest as well as connecting with other mothers.
Postpartum Depression on the other hand, is often treated through psychotherapy, medication or a combination of both.
Psychotherapy
Psychotherapy, also known as talk therapy, is a form of treatment that involves talking with a trained mental health professional such as a psychologist. Therapy allows a mother with PPD to find ways to cope, set goals realistically and overall maintain a positive outlook. In some cases, couples therapy may be helpful for couples whose relationship is strained.
Medication
In severe cases of Postpartum Depression, a psychiatrist may prescribe medication to help with the depression. Antidepressants used during breastfeeding have few side-effects. In many cases, the benefits of the medication far outweigh the little risk of side-effects. The psychiatrist will work together with the mother to get the most ideal medication.
Support Groups
In addition to psychotherapy and medication, support groups can also be an avenue to recovery from Postpartum Depression. Support groups are structured meetings for those living with PPD. The groups are facilitated by a mental health care provider, and typically cover different topics.
These support groups offer a safe space for moms to share their experiences, encourage and comfort each other. The inclusivity of the groups helps mothers know that they are not alone in their experiences.
Postpartum Depression is treatable, and moms who get professional help go on to make a full recovery. For any mom who feels that they could be suffering from PPD or any other mental illness, it is important to remember that you are not alone, and that it is not your fault.
REMEMBER: Tunza Mama carries out a mental health assessment for the new mom with our birth preparation and postpartum packages which you can sign up for here. This, as part of our collective effort to improve maternal health outcomes.
Resources
American Pregnancy Association. (2015, 08). Baby Blues. Retrieved 04 25, 2019, from American Pregnancy Association: https://americanpregnancy.org/first-year-of-life/baby-blues/
Clark, R., Tluzeck, A., & Wenzel, A. (2003). Psychotherapy for Postprtum depression: A Preliminary Report. American Journal of Orthopsyhciatry, 441-450.
Postpartum Depression. (2019, 01 24). Postpartum Depression Support Grpups. Retrieved 04 26, 2019, from Postpartum Depression: https://www.postpartumdepression.org/support/groups/
Postpartum Support International. (2019). Depression During Pregnancy and Postpartum. Retrieved 04 25, 2019, from PSI: https://www.postpartum.net/learn-more/depression-during-pregnancy-postpartum/



